SEOUL, South Korea – A groundbreaking study conducted by a research team at Gangnam Severance Hospital has unveiled a new index designed to predict the risk of adverse events in elderly patients undergoing colonoscopy. This innovative tool aims to enhance patient safety by providing healthcare professionals with a quantifiable measure of potential complications such as bleeding, perforation, and systemic adverse events, which are more prevalent in older individuals due to age-related physiological decline.
The research, led by Professor Chun Jae-young and Professor Kim Min-jae of the Division of Gastroenterology at Gangnam Severance Hospital, was recently published in the international journal Gut and Liver. The findings are expected to significantly improve pre-procedural risk assessment and shared decision-making for colonoscopies in the elderly population.
The Need for a Predictive Tool
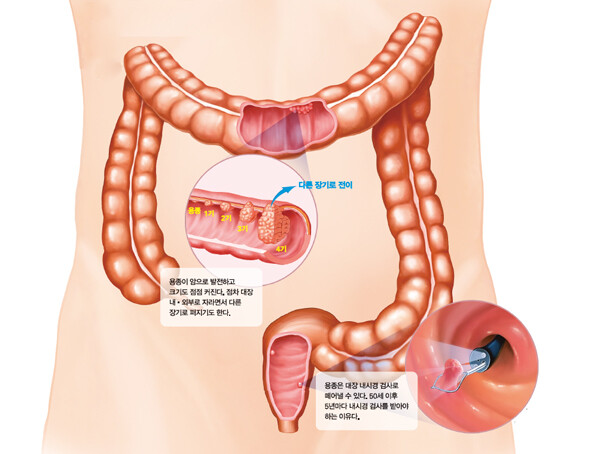
Colonoscopy is a crucial diagnostic and screening procedure for early detection of colorectal cancer and polyps. However, for patients aged 60 and above, the benefits must be carefully weighed against the increased risk of complications. Reduced physical function, pre-existing comorbidities, and the use of certain medications can all contribute to a higher likelihood of post-procedure adverse events. Until now, a standardized and objective method for predicting these risks has been largely absent, often leading to a blanket restriction of colonoscopies for the elderly based solely on age.
"In the past, colonoscopies were often restricted for elderly patients simply due to their age," stated Professor Chun Jae-young. "However, actual adverse events are more closely linked to other factors than just age. This objective index will help both medical professionals and patients and their guardians in determining the course of treatment."
Study Design and Methodology
The research team conducted a retrospective observational study, tracking 8,154 patients aged 60 or older (average age 67.9 years) who underwent colonoscopy between 2017 and 2022. Adverse events were defined as emergency room visits or unplanned hospitalizations within 30 days of the colonoscopy procedure.
To quantify the risk of adverse events, the researchers developed a comprehensive scoring system that incorporated several key factors:
Frailty Index: This index was devised based on individual patient blood test results and vital signs, reflecting the patient's overall physical resilience.
Medication Score: Points were assigned for the use of specific medications, particularly antiplatelet agents (e.g., aspirin) and anticoagulants, known to increase the risk of bleeding. For instance, a patient taking aspirin would receive 1 point, while a patient with a moderate frailty index would receive 2 points.
Patients were then categorized into three risk groups based on their total score: low-risk (0 points), intermediate-risk (1-3 points), and high-risk (4-6 points).
Key Findings: A Clear Correlation Between Score and Risk
The study revealed that 1.4% (114 out of 8,154 patients) experienced an adverse event within 30 days of the procedure. The analysis demonstrated a clear correlation between the developed index and the incidence of complications:
Medication Impact: The use of antiplatelet agents and anticoagulants was independently associated with an increased risk of adverse events.
Frailty and Complications: Patients with intermediate or high frailty index scores exhibited a higher incidence of adverse events compared to those with low scores.
Combined Score Validation: The final combined score, incorporating both the frailty index and medication scores, strongly correlated with the likelihood of adverse events.Low-risk group: 0.3% adverse event rate.
Intermediate-risk group: 2.2% adverse event rate.
High-risk group: 10.7% adverse event rate.
These findings indicate a significant increase in adverse event possibility with higher scores: the intermediate-risk group had an 8.4 times higher chance of complications compared to the low-risk group, while the high-risk group faced a staggering 45 times higher risk.
Validation and Future Implications
To further validate their findings, the research team applied the same analytical method to 9,154 colonoscopy procedures from two other medical institutions, observing similar results. This external validation strengthens the reliability and generalizability of the developed index.
The introduction of this objective and quantifiable risk assessment tool marks a significant advancement in patient care for elderly individuals undergoing colonoscopy. By providing healthcare professionals with a clearer picture of a patient's individual risk profile, the index will facilitate more informed decision-making regarding the appropriateness of the procedure, necessary pre-procedural adjustments, and post-procedural monitoring. This will ultimately contribute to enhanced patient safety and improved outcomes in the growing elderly population.
[Copyright (c) Global Economic Times. All Rights Reserved.]